The FDA's Reversal On uniQure's Gene Therapy For Huntington's Is a Disaster For Medical Innovation
The FDA’s new restrictive approach to rare disease therapies undermines confidence in regulatory consistency and impedes medical progress. After AMT-130 reduced disease progression by 75% in a phase I/II study, the agency’s reversal threatens to delay a breakthrough.

Disclosure: The author holds beneficial long positions in uniQure N.V. (NASDAQ: QURE) and ClearPoint Neuro, Inc. (NASDAQ: CLPT). This article is provided for informational and educational purposes only and is not financial advice. Although the author is a Medical Doctor, this content represents a personal opinion regarding the company’s science and market potential and is not medical advice, a diagnosis, or a treatment recommendation. The author receives no compensation for this article and has no business relationship with the company mentioned. Please see the full "Legal Information and Disclosures" section below.
My article, "uniQure’s AMT-130 for Huntington’s Is One Giant Leap for Medicine," published on September 29, hasn’t aged well, given that the FDA appears to have reversed its stance on approving innovative treatments for rare diseases. Despite this disastrous turn, I increased my positions in uniQure (NASDAQ: QURE) and ClearPoint Neuro (NASDAQ: CLPT) last week. Here, I will explain why I remain skeptical that this FDA turnaround will hold.
Huntington’s disease is a hereditary, relentlessly progressive disorder caused by a CAG repeat expansion in the HTT gene. This mutation results in the accumulation of a toxic mutant protein that ultimately destroys neurons. The disease is characterized by a triad of motor, cognitive, and psychiatric deterioration, often described as combining the symptoms of ALS, Parkinson’s, and Alzheimer’s. Symptoms typically manifest in prime adulthood, leading invariably to death within 10 to 30 years of onset. Approximately 40,000 Americans are currently symptomatic. Because the mutation is autosomal dominant, each child of an affected parent faces a 50 percent chance of inheritance. Until now, medical intervention has been limited to symptom management, with no available disease-modifying treatments.
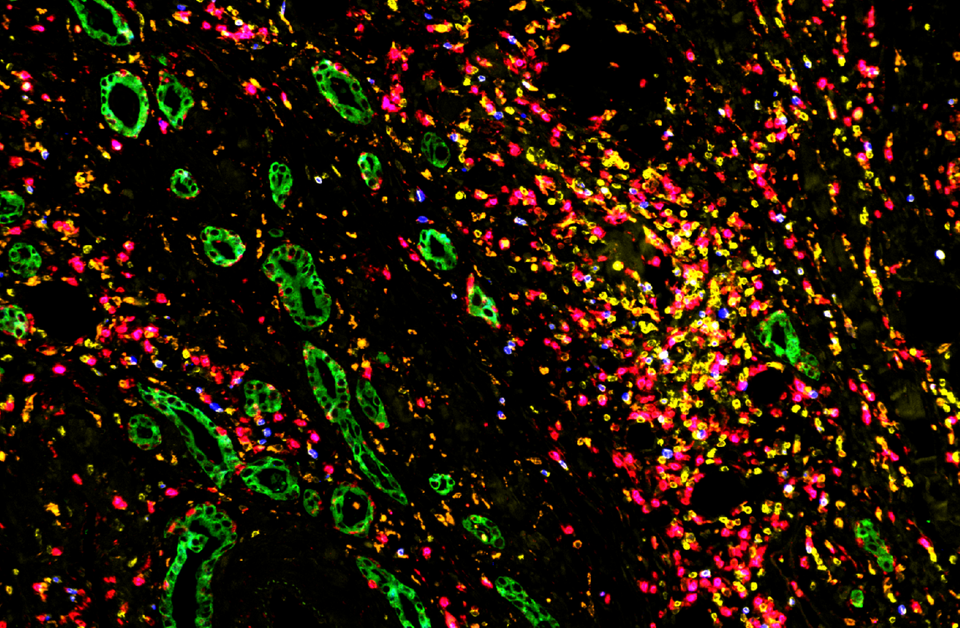
AMT-130, a novel gene therapy by the Dutch biotech company uniQure, changed this. The Phase I/II results, published on September 24, showed that patients receiving the high-dose therapy demonstrated a 75 percent slowing of disease progression compared to natural history cohorts. Professor Sarah Tabrizi, a leading Huntington’s researcher, said the therapy could give patients "decades of good quality life" that would otherwise be lost. Equally important, biological markers mirrored the clinical benefit. Treated patients showed lower levels of neurofilament light (NfL), a protein that reflects neuronal injury, in their cerebrospinal fluid. In untreated Huntington’s patients, these levels typically rise over time, indicating continued brain cell loss. The data suggested that AMT-130 was actually preserving neurons. One neurologist described the findings as "some of the most compelling in all of neurodegenerative disease" after decades of failed attempts. In short, AMT-130 became the first therapy to show that Huntington’s disease can be meaningfully slowed, a true game-changer for a condition long considered untreatable.
AMT-130 is a sophisticated gene therapy administered via an intricate neurosurgical procedure, using equipment developed by the California-based medical technology company ClearPoint Neuro. In a single operation, neurosurgeons infuse a harmless adeno-associated virus (AAV) vector into critical brain regions affected by Huntington’s disease, such as the striatum. This vector carries a custom microRNA payload designed to silence the mutant huntingtin gene. In effect, it reprograms neurons to stop producing the toxic protein that drives the disease. Because the genetic modification is long-lasting, a single treatment could potentially deliver a lasting benefit, stopping the neurodegenerative process at its root. Remarkably, three years into the trial, none of the treated patients have required re-dosing, and their clinical improvements have persisted.
Given these extraordinary results, uniQure moved swiftly toward regulatory approval. Throughout AMT-130’s development, the FDA had always been supportive. The agency granted the therapy Regenerative Medicine Advanced Therapy (RMAT) designation in 2024 and then Breakthrough Therapy designation in April 2025 to expedite its review. In prior communications, the agency had indicated that the Phase I/II data, when compared to robust external controls, could potentially support an application under the Accelerated Approval pathway.
However, on November 3, 2025, uniQure disclosed an abrupt and significant shift by the agency. In a pre-Biologics License Application (BLA) meeting, the FDA reversed its prior stance. UniQure now believes the agency "no longer agrees that data from the Phase I/II studies of AMT-130 in comparison to an external control, as per the prespecified protocols and statistical analysis plans shared with the FDA in advance of the analyses, may be adequate to provide the primary evidence in support of a BLA submission".
This decision, described by uniQure as a "key shift from prior communications," effectively closed the door on the planned BLA filing in early 2026, likely necessitating further, lengthy trials. UniQure’s CEO Matt Kapusta expressed astonishment, noting that as recently as late 2024, the FDA had agreed that the Phase I/II data using an external control "may serve as the primary basis for a BLA submission under the Accelerated Approval pathway." That pathway is now being dismantled. Kapusta said the company is "truly disappointed for people living with HD, who have no disease-modifying treatment options for this devastating disease." Instead of filing for approval in early 2026 as planned, the company must "urgently engage" with the FDA to determine what further trials or analyses are demanded. In plain terms, regulators are tapping the brakes on a life-saving therapy for a terrible disease with no alternative, a delay that patients and their families can ill afford.
This arbitrary reversal directly contradicts explicit written guidance the agency provided just one year prior. As CEO Matt Kapusta stated during uniQure's Q3 2025 earnings call on November 10: “I can confirm that in our November 2024 multidisciplinary meeting with the FDA and the written comments that we received, the FDA stated that the data from the Phase I/II study in comparison to an external control may serve as the primary basis of a BLA submission.”
Furthermore, the agency had confirmed that the composite UHDRS "would be considered an acceptable intermediate clinical endpoint to support accelerated approval" (The Unified Huntington's Disease Rating Scale is a scale to assess the clinical performance of patients with Huntington's and was the study's primary endpoint). The methodology for the external control, using rigorous propensity score matching against the large Enroll-HD dataset, had also been discussed in detail with the FDA in April 2025. As CMO Walid Abi-Saab noted, the company performed numerous sensitivity analyses that were previously agreed upon with the agency, and "across a variety of these analyses, the results were very consistent, demonstrating the robustness of these findings." The FDA appears to have challenged not the data itself, but the foundational agreement on how that data would be evaluated.
The problem lies in the FDA’s new fixation on conventional trial design over pragmatic evidence generation. While randomized controlled trials (RCTs) are the gold standard, they are neither universally applicable nor always ethical. In the case of AMT-130, a traditional placebo control would necessitate a sham neurosurgical procedure, an invasive intervention without therapeutic intent.
However, such rigid standards do not exist in much of modern medicine. Just an example from surgical oncology: no randomized, sham surgery controlled trial has ever been conducted to "prove" that surgical resection of upfront resectable pancreatic cancer improves survival versus chemotherapy alone. Omitting surgery in the control arm would consign those patients to near certain death, an experiment no ethics board could approve. We know from decades of data that surgery combined with adjuvant chemotherapy is the sine qua non for any chance of long term survival in pancreatic cancer.
In the case of Huntington's, could we justify letting half the patients undergo a neurosurgical sham procedure in the name of scientific rigor, while the other half receive a therapy that enormously slows the disease? It would be very difficult. This is precisely why, in such cases, studies can utilize external control groups derived from natural history registries, especially when no alternative therapy is available for comparison. The FDA possesses the authority to accept externally controlled trials, particularly when ethical concerns preclude the use of a placebo arm. The sudden assertion that these comparisons lack sufficient rigor suggests the FDA is now demanding something which could delay access to AMT-10 for several years, if not forever: a new double blind, sham surgery controlled trial.
It’s worth recalling the words of philosopher Paul Feyerabend, who wrote in his 1975 work Against Method that "science is an essentially anarchistic enterprise: theoretical anarchism is more humanitarian and more likely to encourage progress than its law-and-order alternatives." The agency seems to forget that medicine often requires acting on the best available evidence, especially when the alternative is certain decline and death. Or as the great Canadian physician Sir William Osler once put it: "Medicine is a science of uncertainty and an art of probability."
The FDA’s handling of AMT-130 is not an isolated incident but reflects a broader, concerning trend in the regulation of rare disease therapies. This rigidity stands in direct contradiction to the intent of Congress, which has explicitly empowered the FDA to exercise regulatory flexibility, notably through the 21st Century Cures Act, which encourages the use of innovative trial designs and real world evidence.
This new approach against novel therapies for rare diseases is occurring against a backdrop of significant internal instability at the FDA, which culminated in the abrupt resignation of Center for Drug Evaluation and Research director Dr. George Tidmarsh in early November 2025, amid “serious concerns about his personal conduct”. His departure coincided with a lawsuit alleging Tidmarsh used his FDA position to pursue a personal vendetta, making defamatory statements about another company’s drug that erased hundreds of millions in market value. In the opinion article "The FDA’s Meltdown Escalates," published in the Wall Street Journal on November 6, the FDA's current state was even called an "embarrassment."
While discussions of breakthrough therapies invariably raise concerns about cost, the value proposition must be considered holistically. Gene therapies carry high upfront costs, but these are often one-time treatments that offset decades of disability and intensive care expenses. For example, the UK’s National Health Service currently pays £2.6 million (≈$3.5 million) per patient for a gene therapy curing hemophilia B—and still deems it cost-effective given the lifetime benefits.
For Huntington’s, a disease that strikes people in their prime and devastates families across generations, even a multi-million-dollar therapy could be a bargain relative to the incalculable human and economic toll of the illness. Organizations that assess medical value frequently find that even multi-million-dollar gene therapies for severe diseases meet common thresholds for cost-effectiveness due to their transformative long-term benefits. For Huntington’s, which strikes individuals in their productive years, the economic and societal value of preserving function is substantial.
At stake is also the broader question of whether the United States (and the West broadly) will maintain its global leadership in biomedical innovation, or whether excessive skepticism and procedural inertia will be allowed to impede scientific progress. The development of AMT-130, from lab concept to human trial, is a triumph of ingenuity, funded and executed by Western scientists and companies, with crucial support from patients and advocacy groups. It proves that we can solve the unsolvable, that we haven’t run out of moonshots. Crucially, innovations pioneered in challenging areas often create new platforms and fundamental insights that ultimately benefit the practice of medicine as a whole.
From a policy standpoint, such breakthroughs should be facilitated through clear regulatory pathways, not hindered by shifting requirements. Every delay sends a negative signal to researchers and investors, suggesting that even scientifically successful, high risk endeavors may face prohibitive regulatory uncertainty. It would represent a significant setback if, after science has delivered a potential therapy for Huntington’s, an overly cautious regulatory framework obstructs its path to patients and discourages future ambitious research. It’s time to reverse course. Lives depend on it.
All of this makes it hard for me to believe that a historic breakthrough like AMT-130 will ultimately fail due to law-and-order regulation. President Donald Trump encouraged Americans in his inaugural address on January 20 to "dream boldly," with "ambition" as "the lifeblood of a great nation" that will "manifest destiny into the stars, launching American astronauts to plant the Stars and Stripes on the planet Mars." Ambition is also the core of scientific and medical innovation, and being able to treat the formerly untreatable is its own kind of Mars landing.
Follow me on X for frequent updates (@chaotropy).
Legal Information and Disclosures
General Disclaimer & No Financial Advice: The content of this article is for informational, educational, and entertainment purposes only. It represents the personal opinions of the author as of the date of publication and may change without notice. The author is not a registered investment advisor or financial analyst. This content is not intended to be, and shall not be construed as, financial, legal, tax, or investment advice. It does not constitute a personal recommendation or an assessment of suitability for any specific investor. Readers should conduct their own independent due diligence and consult with a certified financial professional before making any investment decisions.
Medical Disclaimer: Although the author possesses a medical background, the information presented here regarding medical technologies, clinical trials, or pharmaceutical mechanisms is strictly for the purpose of educational discussion and general commentary regarding the underlying science. It does not constitute medical advice, diagnosis, or treatment recommendations, nor does it establish a physician-patient relationship. Readers should never disregard professional medical advice or delay in seeking it because of something read on this website. Always consult a qualified healthcare provider regarding any medical condition.
Accuracy and Third-Party Data: Market trends, clinical trial data, and performance metrics referenced in this article are sourced from independent third parties. While the author believes these sources to be reliable, the completeness, timeliness, or correctness of this data cannot be guaranteed. The author assumes no liability for errors, omissions, or the results obtained from the use of this information.
Disclosure of Interest: The author holds beneficial long positions in uniQure N.V. (NASDAQ: QURE) and ClearPoint Neuro, Inc. (NASDAQ: CLPT). The author reserves the right to buy or sell these securities at any time without further notice. The author receives no direct compensation for the production of this content and maintains no business relationship with the companies mentioned.
Forward-Looking Statements & Risk: This article contains forward-looking statements regarding regulatory outcomes (such as FDA decisions), clinical results, and market potential. These statements are predictions based on current expectations and are subject to significant risks and uncertainties. Investing in biotechnology and pharmaceutical securities involves a high degree of risk, including the potential for total loss of principal. Past performance is not indicative of future results.
Copyright: All content is the property of the author. This article may not be copied, reproduced, or published, in whole or in part, without the author's prior written consent.